Highlighted for its proven efficacy on certain respiratory diseases, vitamin D has received particular attention since the emergence of Covid-19. Observational studies and a larger systematic review on SARS-Cov-2* have linked vitamin D deficiency to a higher risk of testing positive for SARS-CoV-2 and developing severe forms of COVID-19(1-4). Nevertheless, co-morbidities such as diabetes, cardiovascular and respiratory diseases as well as obesity [3-6] should not be overlooked as they also play a very important role.
Synthesis of vitamin D
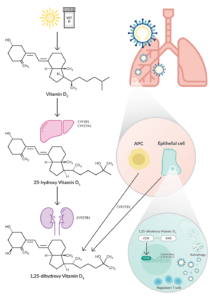
Vitamin D3 is obtained from certain dietary sources and by the action of UVB on 7-dehydro cholesterol in the skin. Hydroxylation of vitamin D3 in the liver produces 25-hydroxy vitamin D3, the major circulating form of vitamin D, which is an intermediate in the pathway leading to the production of 1,25-dihydroxy vitamin D3, the most active form on vitamin D3 receptors.
Antigen-presenting cells (APCs) and epithelial cells can also synthesize 1,25-dihydroxy vitamin D3 via 1α-hydroxylase/CYP27B1, which is regulated by an immune stimulus. For example, human macrophages stimulated by recognition of the M. tuberculosis Toll-like receptor induce CYP27B1 and vitamin D receptor expression(5). 1,25-dihydroxy vitamin D3 signals via the vitamin D receptor (VDR), which is widely expressed in epithelial tissue and immune cells.
Role of vitamin D
Considered more like a hormone than a vitamin, vitamin D plays multiple roles. In addition to its vital role in bone health, vitamin D acts on antimicrobial peptide expression and supports the anti- inflammatory process that supports immune defense. It acts directly on the conversion of angiotensin-enzyme 2 (ACE2), which serves as a cell surface entry receptor for SARS-CoV-2.
Vitamin D can directly induce the expression of the antimicrobial peptide cathelicidin, as well as β- defensin-2 genes(6). Cathelicidin induces a variety of proinflammatory cytokines, stimulates neutrophil, monocyte, macrophage, and T-cell chemotaxis at the site of infection, and promotes the elimination of respiratory pathogens by inducing apoptosis and autophagy of infected epithelial cells. β-Defensin- 2 stimulates the expression of antiviral cytokines and chemokines involved in the recruitment of monocytes, macrophages, natural killer cells, neutrophils and T cells.
Another property of 1,25-dihydroxy vitamin D3 is the promotion of autophagy, in which viral particles are conditioned for lysosomal degradation and subsequent antigen presentation for adaptive antiviral immune responses(7).
1,25-dihydroxy vitamin D3 also exerts inhibitory and anti-inflammatory actions on the adaptive immune system, decreasing dendritic cell maturation and suppressing type 19 helper T cell responses. Dendritic cells treated with 1,25-dihydroxy vitamin D3 can also induce regulatory T cells, which may play a role in preventing a cytokine storm caused by viral infection.
Vitamin D and ACE2
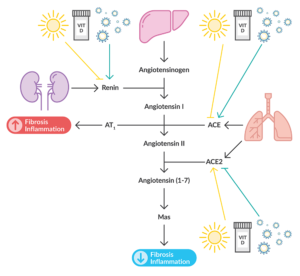
The main entry point into SARS-CoV-2 cells, the ACE2 receptor is part of the renin-angiotensin system. Once the virus attaches to human ACE2 via its spike glycoprotein, it reduces the expression of ACE2, leading to excessive production of angiotensin (Ang) II. This overproduction results in the growth and proliferation of pulmonary fibroblasts causing pulmonary inflammation by increasing free radicals and pro-inflammatory cytokines leading to the development of lung damage. The balance between ACE2 and ACE appears to be crucial because ACE2 counteracts the effects of ACE by hydrolyzing angiotensin II to angiotensin (1-7), thereby activating the MAS receptor pathway and resulting in an anti-inflammatory effect.
Vitamin D activates the ACE2/Ang (1-7)/Mas receptor pathway while inhibiting ACE/Ang II/AT1 activity.11 It also acts as a negative modulator of the renin-angiotensin system by inhibiting renin expression and generation. Thus, vitamin D may provide protection against lung injury.
What do the researchers think?
From four databases, the researchers identified 31 peer-reviewed observational studies. The points of interest identified were:
- Mortality
- Admission to intensive care
- Vascular and non-invasive inventilation
- Hospitalization and length of stay
The main conclusion of these studies is that while there is a correlation between a c(VitD)** <20ng/ml and an increased risk of the disease. This finding is not statistically significant(8). While calcifediol supplementation may have a protective effect on COVID-19-related ICU admissions, no sufficiently relevant studies have shown a causal relationship. The current use of high doses of vitamin D in COVID-19 patients is not based on solid evidence. The protocols of these studies were considered unreliable or limited in number of patients. Trials are underway to determine the efficacy, desirable doses, and safety of vitamin D supplementation to prevent and treat the health effects of COVID-19.
You have needs concerning the study of the protective mechanisms of vitamin D?
Advion Interchim Scientific offers you several products:
- Vitamin D & analogues
- Vitamin D Assay Kits
For any need concerning reagents related to vitamin D, please contact us by email.
* SARS-Cov-2: Severe Acute Respiratory Syndrome
** c(VitD): Vitamin D concentration
References :
- Meltzer, D.O., Best, T.J., Zhang, H., et al. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw. Open 3(9), e2019722 (2020).
- Meltzer, D.O., Best, T.J., Zhang, H., et al. Association of vitamin D levels, race/ethnicity, and clinical characteristics with COVID-19 test results. JAMA Netw. Open 4(3), e214117 (2021).
- Pereira, M., Damascena, A.D., Azevedo, L.M.G., et al. Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. (2020).
- Ricci, A., Pagliuca, A., D’Ascanio, M., et al. Circulating vitamin D levels status and clinical prognostic indices in COVID-19 patients. Respir. Res. 22(1), 76 (2021).
- Liu, P.T., Stenger, S., Li, H., et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 311(5768), 1770-1773 (2006).
- Wang, T.-T., Nestel, F.P., Bourdeau, V., et al. Cutting edge: 1,25-Dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J. Immunol. 173(5), 2909-2912 (2004).
- Wang, J. Beclin 1 bridges autophagy, apoptosis, and differentiation. Autophagy 4(7), 947-948 (2008).
- Bassatne, A., Basbous, M., Chakhtoura, M., et al. The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis. Metabolism 119, 154753 (2021).










This is an embarrassing article. You need to replace your team of scientists. They are missing most of the Vit D data. Please remove it before you further embarrass your company.
Thank you for your feedback. Our article is not intended to explore this complex subject in depth. It is meant to present the main elements and give the readers the desire to go and look for additional information by themselves. Given the research you are doing, we can understand your frustration. If you feel this way, we are open to a discussion to better understand your point of view and potentially complete our article. Please feel free to contact the team in charge of this topic at biosciences@advion-interchim.com.