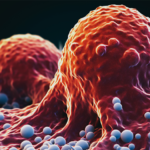
Since December 2019, the new SARS-Cov-2 coronavirus has spread around the world. In the most cases, this virus is fortunately benign with no sequelae. Fever, fatigue, dry cough and loss of smell or taste are the main symptoms. Unfortunately, in 1 to 2 out of 10 cases, the virus is insidious, with some patients’ condition suddenly deteriorating at the beginning or during the second week. This life-threatening deterioration is often the result of a runaway inflammation process, known as “cytokine storm”.
A bit of history
Although the phenomenon of excessive or uncontrolled release of pro-inflammatory cytokines is well known, the term “cytokine storm” emerged in 1993 in the description of graft-versus-host disease (GVHD). Researchers have been influenced by the recent war called “Desert Storm”. The term was later widely popularized in relation to infectious and non-infectious diseases, particularly in the context of infection with the H5N1 avian influenza virus [Tisoncik 2012]. The occurrence of a “cytokine storm” has been suggested as an explanation for the devastating nature of the 1918 influenza pandemic. This inflammatory disruption has been blamed for other viruses, including SARS Coronaviruses in 2003 and MERS-Cov, and now SARS-Cov2.
Symptoms and Cytokine Shock
Cytokine Storm Syndromes (CSS) are a group of disorders that are often inflammatory in nature. The main symptoms of a cytokine storm are high fever, swelling and redness, extreme fatigue and nausea. In some cases, the immune response can be fatal. In particular, the symptoms of Covid19 are fever, dry cough and dyspnea that require monitoring, but also joint pain and digestive signs.
Cytokine shock can cause significant tissue and organ damage. In the case of Covid-19, if a cytokine storm occurs in the lungs, for example, fluids and immune cells such as macrophages can accumulate and eventually block the airways, eventually leading to death. This phenomenon is called acute respiratory distress syndrome..
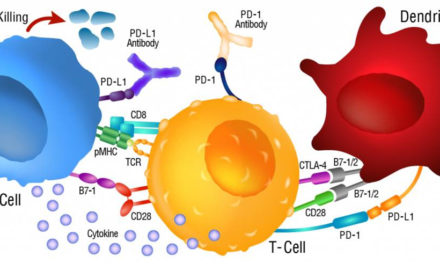
In covid-19, interleukin 6 appears to be the key mediator of cytokine shock, but interleukin 1 (IL-1β) and tumour necrosis factor (TNFα), which IL6 induces, also play a large role. In particular, the role of chemo-attractive cytokines (chemokines) has recently been discussed [Coperchini 2020-05]. In response to this cytokine hyperstimulation, the level of CD4 T lymphocytes decreases while CD8 T lymphocytes increase.
The balance of CD4/CD8 markers is considered as an important prognosis of the disease. Elevation of serum IL-6 is thought to be a good marker for the pejorative course of COVID-19 [Zhang 2020]. Elevated ferritin has been reported to be a good diagnostic indicator of cytokine shock.
Unlike other viral infections, the prevalence or extent of inflammation in cases of COVID-19 is not associated with treatments involving anti-cytokine and anti-inflammatory agents (immunosuppressants, NSAIDs, JAK kinase inhibitors) [Van Hemelrijck,2020].
Numerous clinical trials targeting inflammatory pathways are underway. Some are promising, such as blocking IL6 through the use of tocilizumab. Research is also targeting IL-6 expression activators IL-1β and TNFα [Zhan 2020-05].
Interchim® offers a selection of kits for the assay of the different cytokines and chemokines mentioned. To study the relative variations between cytokines, discover the MEK1008 kit and other multiplex kits dedicated to the quantification of pro-inflammatory cytokines in blood, plasma and serum.
| Description | Référence |
| Multiplex ELISA Kit For Human Cytokine – Inflammation (9-plex), IL-1α, IL-1β, IL-4, IL-5, IL-6, IL-10, IL-17, IFNγ, TNFα | MEK1008 |
| Multiplex ELISA Kit For Human Cytokine – Stripwells (16-plex), IL-1α, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-13, IL-15, IL-17, IL-23, IFNγ, TNFα, TNFβ | MEK1001 |
| Multiplex ELISA Kit For Human Cytokine – Screen (16-plex), IL-1α, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-13, IL-15, IL-17, IL-23, IFNγ, TNFα, TNFβ | MEK1005 |
| Multiplex ELISA Kit For Human Cytokine HS Screen (15-Plex), IL-1α, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12p70, IL-13, IL-15, IL-17, IL-23, IFNγ, TNFα, TNFβ | MEK1007 |
| Multiplex ELISA Kit For Human Cytokine Panel 1 (6-Plex), IL-1β, IL-6, TNFα, IFN-γ, IL-1α, IL-10 | MEK1010 |
| Multiplex ELISA Kit For Human Cytokine Panel 2 (6-Plex), IL-6, IL-8, TNFα, IFN-γ, IL-4, IL-10 | MEK1012 |
| Multiplex ELISA Kit For Human Cytokine (4-Plex), IL-6, TNFα, IFN-γ, IL-10 | MEK1014 |
Know more:
- Find other reagents dedicated to research and diagnosis of Covid-19:
– by downloading our special brochure
– by consulting our dedicated pages - Contact us: interbiotech@interchim.com