Business insider-
‘Crazy hours, short nights’: The inside story of how a buzzy biotech upstart developed a potential coronavirus vaccine in record time
Mar 6, 2020, 5:15 PM
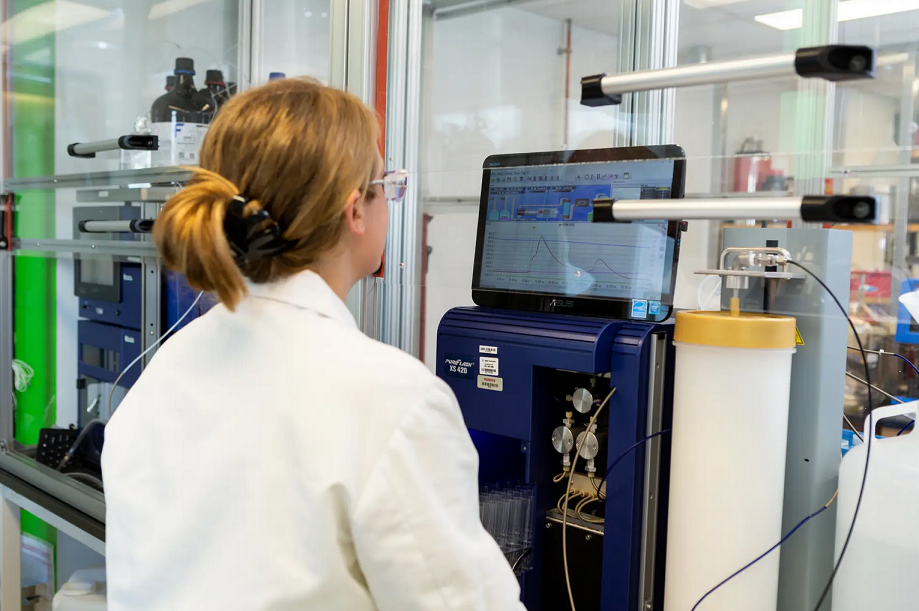
Tablets allow Moderna employees to monitor daily operations. Moderna
- The $10 billion biotech Moderna developed a potential coronavirus vaccine in record time, zooming past Big Pharma competitors.
- Stephane Bancel, the company’s CEO, sat down with Business Insider to discuss the technology platform that drove its speed and how the company hopes to pioneer a new way of developing vaccines.
- “The speed is one dimension, but the piece that excites me the most about this technology is we can do vaccines that cannot be done using traditional technology,” Bancel said.
- The potential coronavirus vaccine will still require at least 12 to 18 months of testing in humans to determine if it’s safe and works to prevent the virus, according to a top US health official.
- Here’s the inside story of how Moderna went from waiting for the virus to be sequenced to shipping a vaccine in 42 days.
- Visit Business Insider’s homepage for more stories.
NORWOOD, Massachusetts — Stephane Bancel was vacationing in the south of France with his family when he first read about the virus.
It was early January when the biotech executive saw a Wall Street Journal article describing a “mystery virus outbreak” in central China. He sent an email from his iPad about the story to Dr. Barney Graham, the deputy director of the Vaccine Research Center at the National Institutes of Health.
Graham said the agency didn’t know what the virus was yet. A few days later it did: a novel coronavirus. Bancel asked the NIH leader to let him know when they had the virus’ genetic sequence. His company, Moderna, was ready to get to work.
In the weeks since, the virus has spread across the globe, weighed on financial markets, and killed more than 3,300 people. In that same period, about 100 employees at Moderna, about one-tenth of the company’s workforce, worked around-the-clock to develop a coronavirus vaccine.
“They did what they had to do to get things done,” Bancel, Moderna’s CEO, said in an interview with Business Insider, adding that the period was full of “crazy hours, short nights.”
The biotech shipped the first batches of a vaccine to the NIH on February 24, just 42 days after it received the virus’ genetic sequence.
Moderna CEO Stephane Bancel. Steven Ferdman/Getty Images
Now, under the brightest possible spotlight as the outbreak spreads, Moderna is challenging the lengthy and costly process of vaccine development. The company has never before brought a vaccine to market, and a victory would help establish its platform as a new type of medicine.
Early human data from other Moderna vaccines released in 2019 helped show that its approach works, Alan Carr, a Needham analyst, said in an interview. But Carr said the company still faces risks in development, as it has yet to start any late-stage clinical testing — the final step before gaining regulatory approval for vaccines and medicines.
It will take at least 12 to 18 months to know if Moderna’s vaccine — or any others — is safe and effective, Anthony Fauci, the longtime leader of the NIH’s infectious-disease unit, has repeatedly said.
The first clinical trial kicks off just as some much larger drugmakers have put out only timelines to get to that stage. Johnson & Johnson, the largest healthcare company, hopes to start a vaccine clinical trial in November. The French pharma giant Sanofi expects to start a coronavirus-vaccine study in early 2021.
With the world watching, Moderna didn’t just outpace its Big Pharma rivals, which dwarf the Massachusetts biotech in size and resources, it lapped history. It took more than 10 times as long to go from genetic sequence to vaccine candidate in the case of the 2002-03 SARS outbreak.
But given the time it takes to determine if a vaccine works, the vaccine would be a longer-term solution. With the potential for the virus to reemerge in future seasons, a coronavirus vaccine still holds immense public-health value, research-and-development experts told Business Insider.
Bancel told us, citing the public-health value, that Moderna would be “very thoughtful” about setting a price.
“There is no world, I think, where we would contemplate to price this higher” than vaccines to prevent other respiratory infections, he added.
The day after US regulators cleared Moderna’s coronavirus vaccine to start human testing, Bancel told Business Insider about his vision for Moderna, which stretches far beyond the coronavirus. With its technology platform, called messenger RNA, Moderna could respond just as quickly to future outbreaks, as well as tackle diseases for which no vaccine exists, like Zika and mononucleosis.
“The speed is one dimension, but the piece that excites me the most about this technology is we can do vaccines that cannot be done using traditional technology,” Bancel said.
“This is where we’re going to change the game completely,” he added, talking about lowering the cost and shortening timelines of vaccine development.
Without a single approved drug or vaccine, Moderna has ridden the potential of its technology into biotech’s top ranks. That first fueled the largest biotech initial public offering in history in December 2018 and now has led Moderna to break the $10 billion valuation mark with a speedy response to this latest outbreak. Its share price has increased about 30% since it went public.
Hartaj Singh, a biotech analyst at Oppenheimer who covers the company, thinks investors are still getting Moderna’s stock at a cheap valuation. Singh said it would be years before investors fully appreciate the value of Moderna’s scientific advances. He compared the company to Genentech, a legendary biotech firm that was a leader in developing antibodies. The Swiss pharma company Roche agreed to buy Genentech for $47 billion in 2009.
Inside Moderna’s labs. Moderna
‘This is not the same game’
The 47-year-old Bancel, dressed casually in jeans and a sweater with elbow pads, politely explained in his French accent a no-handshake policy at Moderna during the outbreak as he stepped into his office at the Cambridge, Massachusetts, headquarters. (We tapped feet instead.)
While most of Moderna’s employees work in Cambridge, the bulk of the work on a coronavirus vaccine happened about an hour away in the small town of Norwood, Massachusetts. The company spent about $110 million on the 200,000-square-foot facility, which opened in 2018 and was once a Polaroid plant.
In a matter of weeks, it became a hotbed for developing a coronavirus vaccine as quickly as possible using Moderna’s genetics-based platform for vaccine development.
At the basic level, vaccines work by giving cells a taste of a virus — just enough for our bodies to recognize it as an intruder and pump out antibodies to fight a similar invasion in the future.
For decades, vaccines have traditionally contained a dead or weakened version of the virus itself. Early advances in genetics allowed a vaccine to use just proteins made by the virus. That method was first used in the 1980s to develop a vaccine for hepatitis B.
Moderna is also working to develop personalized cancer treatments that are custom-crafted for each patient. Moderna
Moderna has gone a step further back: Instead of using viruses or proteins, the platforms works with just the genetic material. The biotech is focused on messenger RNA (mRNA) — the genetic material from DNA that makes proteins.
Because of the speed of its platform, Moderna has had the potential to fight infectious-disease outbreaks from the company’s beginnings in 2011.
Part of the company’s speed in responding to the coronavirus came from it tapping existing research relationships, Bancel said. Moderna has been working with the NIH for a couple of years on two RNA viruses called Nipah and MERS. MERS, or Middle East respiratory syndrome, is also caused by a coronavirus.
The purpose of the collaboration was obvious: “Chasing a pandemic is really hard if you’ve done no biology work, so let’s start to work on a few dangerous strains to get moving,” Bancel said.
In November, top NIH vaccine officials Dr. John Mascola and Graham visited Norwood and discussed the potential to advance some of that research work in 2020 with Moderna.
Then the coronavirus began spreading in China, just a few weeks after that visit. On January 10, scientists from Fudan University in Shanghai posted the genomic sequence of the coronavirus.
Teams at the NIH and Moderna both pored over that data, hunting for targets. Just three days later, both sides convened — they had independently arrived at the same targets for a prospective vaccine.
That preclinical process of finding and selecting a target can take years for traditional vaccines, Bancel said, instead of three days at Moderna.
“This is not the same game,” Bancel said. “We never saw the virus. We don’t need to see the virus. What we need is the genetic instruction of the virus.”
The Moderna team based in Norwood moved quickly: One group of engineers designed the mRNA vaccine candidate, while another group converted an area used for personalized cancer vaccines into a space to pump out the first doses of a coronavirus vaccine.
“There were some changes in the process the team had to test on the fly,” Bancel said, adding that it was the first time the cancer space has been used in this manner.
By February 7, the company had completed a first batch of the vaccine. After a couple weeks of quality testing, Moderna sent the first doses to the NIH on February 24 — 42 days after the virus’ sequencing.
The Norwood facility has little innovations that stack up into a competitive advantage. The labs are paperless, which expedited a documentation process that usually takes weeks or months to produce a clinical batch.
Most of the research space is equipped with what look like security cameras in the corners. These track how researchers move around the space, collecting data that can suggest tweaks to how equipment is mapped out to improve efficiency.
Virtually all the equipment in the lab for personalized cancer treatments is on wheels so that it can be quickly reconfigured into a new layout. Even tiny actions have been sped up, like ordering lab supplies. Buttons are attached to bins that store disposable equipment like gloves. Instead of logging on to Amazon to order more supplies when running low, a researcher can hit the button to trigger an order.
Moderna could make ‘millions’ of doses of coronavirus vaccine, CEO says
Now the NIH will lead clinical testing of the vaccine. The first study has just begun to recruit patients and looks to test three dose levels in 45 healthy adults in the US to see if the vaccine is safe.
Future tests would focus on whether the vaccine works and involve hundreds to thousands of people.
As far as unanswered questions go, the most pressing is if this vaccine will work. Right behind that is what happens next if it is found to be safe and effective. Can a biotech with a fraction of the resources of pharmaceutical giants like J&J and Sanofi produce enough vaccines to make a difference?
Bancel said Moderna’s Norwood plant could make “millions” of doses in a year, if needed, declining to provide a more specific number. So far, the company has made a few hundred doses for the first small clinical trial underway in Washington state.
Juan Andres, the company’s chief technical operations and quality officer, said in a presentation to investors in November that the biotech could make 10 million doses per year of a vaccine for a common virus called cytomegalovirus, or CMV, assuming a 100-microgram dose. At that level, it wouldn’t affect other operations at the plant.
And if the Norwood site were solely focused on pumping out its CMV vaccine, Andres estimated it could produce 100 million doses per year.
In contrast, massive pharmas like J&J and Sanofi have excess capacity to produce hundreds of millions of doses without disrupting other projects, Carr said. The uniqueness of the mRNA platform could pose a challenge to the company when it rapidly scales doses into mass production, with an external manufacturer having to learn that system.
Bancel added that the company was looking into building out more of its Norwood space with equipment to boost its vaccine-production capacity, with the biotech intentionally choosing a facility bigger than they are using to have room to grow into.
Beyond the coronavirus, Moderna is hoping to apply mRNA to many diseases with no approved vaccines, in addition to future outbreaks. The company has seven vaccines in clinical testing for viruses with no approved vaccines, including Zika and the virus that causes mononucleosis, among others.
“We are moving biology to a digital world, where we can work out of a sequence, and we don’t invent a molecule,” Bancel said. Instead, Moderna is tapping nature’s own genetic instructions to do the work.